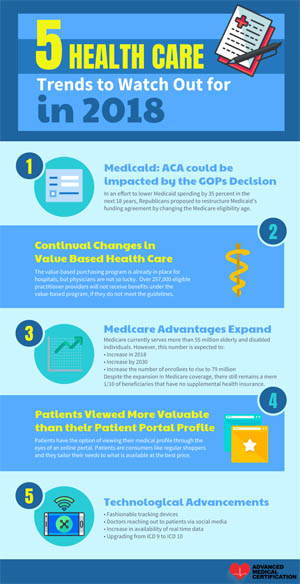
Top 5 Health Care Trends to Watch Out For 2018
OUR HEALTH CARE INDUSTRY IS FACING TRYING TIMES, as new and emerging events take place. The challenges of maintaining health care coverage comes with a price. The Affordable Care Act bill is currently under review as Republicans look to reform Medicaid, Medicare and the Affordable Care Act. These are all government insurance programs which mostly benefit the poor, elderly and underserved. With an outcome nowhere in sight, our government continually faces another uphill battle from hackers, the opioid epidemic and a nationwide “Killer” flu.
 As a result of these challenges, we as a people should look for five major trends to take place in 2018.
As a result of these challenges, we as a people should look for five major trends to take place in 2018.
These trends will cost the American people to demand for justice and reevaluate the systems in place. Insurance comes with a cost, and those who have it are benefiting from:
- Affordable health care
- Proper medical care
- Access to medical care
- Prescription drugs
- Medical supplies
- Rehabilitation
- Dental care
- Well care visits
Fortunately, the list goes on. However, if the ACA is overturned, these services and benefits may change. As the debate continues, everyone is expecting a possible outcome, one that everyone can live with.
1. Medicare: Medicaid-Affordable Act could be impacted by the GOPs Decision to Cut Back
In an effort to lower Medicaid spending by 35 percent in the next 18 years, Republicans proposed to restructure Medicaid’s funding agreement. In December of last year, Paul Ryan—the 54th Speaker of the United States House of Representatives—made a profound statement during the 2017 health reform debate. He stated that the first business of duty for Republicans will be to reduce benefits recipients are entitled to under federal spending programs. What do this mean for individuals relying on Medicare, Medicaid and the Affordable Act Marketplace insurance coverage?
The opposition to the proposal comes from Andy Slavitt, past acting Administrator, who offers some advice on cutting insurance cost. Not everyone is as eager as Paul Ryan and his colleagues to reform Medicaid or make “Deep cuts.” Instead, the Senate should be looking for ways to resolve their differences and stay focused on reaching a solution to maintaining quality health services and benefits for our aging and underserved citizens.
The Republicans toyed with the idea of transforming the Medicaid program into a collaboration, which allows the government to contribute a portion of money towards an elderly person’s health premium. The problem with this theory opens another issue which translates to an increase in health care spending. One possible solution Republicans advanced is one that will affect millions of senior citizens in the United States by changing the Medicare eligibility age. With so many seniors reaching retirement, this theory will certainly put a strain on families and individuals.
2. Continual Changes in Value Based Health Care
Americans can expect more of the same tactics from the Trump Administration when it comes to downplaying Obama Care. Their plan in 2017 was geared towards ending three already planned “Bundled” payment models associated with Medicare. The plan was to scrap a well-needed incentive payment model that would benefit the cardiac rehabilitation health industry. However, the health care industry will continue to thrive in maintaining its path towards improved outcome-based models.
The value-based purchasing program is already in place for hospitals, but physicians are not so lucky. Hospitals serve millions of people on a regular basis, and so do physician offices, clinics and other counterparts of the health care industry, though at a slower pace. Nevertheless, over 257,000 eligible practitioner providers will not receive benefits under the value-based program if they do not meet the guidelines. The industry in question must:
- Show a continual use of the EHR system
- Be certified users of EHR technology; or have their funding cut by one percent.
- Follow Medicare Electronic Prescribing Incentive Program (eRX)
- Comply with the Physician Quality Reporting System (PQST)
Although doctors face penalties when not complying with the Medicare reporting system, they also have an opportunity to fight back. Physicians are allowed to present CMS with a monthly bill for obtaining remote chronic management for qualifying patients.
3. Medicare Advantages Expand in 2018
Good news for individuals 65 years and older who qualify—or might already have—Medicare. According to a recent report on the NCPSSM.org (National Committee to Preserve Social Security & Medicare Facts) website, Medicare currently serves more than 55 million elderly and disabled individuals. However, this number is expected to:
- Increase in 2018
- Increase by 2030
- Increase the number of enrollees to 79 million
Despite the expansion in Medicare coverage, only about one in ten of these beneficiaries lack supplemental health insurance, while the remaining 90 percent carry some type of supplemental coverage. Medicare is one of the largest providers of services for elderly and disabled Americans who meet the age and disability guidelines. The program contains four separate parts, each supporting a different function. While some individuals have only Parts A and B, others might have Part C or D, depending on their needs and qualifications. If the program is canceled, millions of underserved, medically disadvantaged, and elderly people will be left with little or no access to medications, prescription assistance, medical supplies, or hospital coverage. However, no one wants to cut the program, so everyone in D.C. is looking for a mutual agreement that benefits all.
4. Patients Viewed More Valuable than their Patient Portal Profile
Patients now have the option of viewing their medical profiles through an online portal. Like regular shoppers, patients tailor their needs to what is available at the best price. When shopping for online deals, information proves to be an invaluable resource. The health care industry is expected to pay more for value and not just numbers. Hopefully, this approach will encourage health companies to pursue a strategic investment plan that improves the patient experience.
What is a Patient Portal? It is an online website detailing the patient’s experience where one can view:
- Recent and upcoming doctor visits
- Prescription medications
- Lab results
- Immunization records
- Discharge summaries
- Scheduled appointments
- Verified allergies
- Non-emergency medical appointments
- Updated contact information
- Payment options
- Downloadable and printable forms
- Educational pamphlets or materials
The patient portal offers many resources and benefits, accessible 24 hours a day.
5. Technological Advancements Transforming the Entire Health Care Industry
Technology is evolving at an increasingly brisk pace, especially in the health care industry. Now that technology is being used to track patients, what changes can we expect?
Fashionable Tracking Devices
In the United States, more than 70 million individuals wear some type of tracking device to record their physical activities. These devices monitor sleep patterns, calorie intake, miles walked or run, and more. Improved tracking devices will help enhance overall patient care, encouraging patients to participate actively. Good health is a priority, and everyone wants to know where they stand medically.
Doctors Reaching Out to Patients via Social Media
In a world where comparative shopping, social interactions, and personal greetings occur from anywhere, the health care industry is stepping up its game in connecting with patients outside the traditional office setting. This is groundbreaking territory for health care providers—and for patients seeking the best insurance coverage. Although HIPAA and related laws have traditionally limited such interactions, the landscape may change rapidly in 2018 as providers explore innovative ways to improve patient satisfaction.
Increase in Availability of Real-Time Data
Despite improvements in electronic health record systems, some health care facilities still experience gaps in the information needed to provide quality patient care after discharge. To streamline access to essential data, an Enterprise Data Warehouse (EDW) could be the missing link. Such a system would allow both technical and non-technical personnel to access and transfer critical information, potentially saving lives, reducing costs, and expediting patient care.
Upgrading from ICD 9 to ICD 10
When the new ICD coding system was introduced more than 20 years ago, it generated considerable controversy. Today, similar debates continue as the ICD 9 system is upgraded to ICD 10. Although this transition, years in the making, is already underway, health care professionals are expected to start integrating the new system as soon as possible. This change means that coders must learn and use the new coding system. While training and implementation may be challenging and overwhelming for hospitals, doctor's offices, and other facilities, failure to adopt the new codes in a timely manner could have far-reaching consequences. Any mistake in coding can be costly, as codes are essential for billing and claims processing across Medicare, Medicaid, and private insurance. Under the ICD 10 system, coders must learn and apply more than 68,000 diagnostic codes; a recent survey revealed that over 9 percent of physician groups are not yet in compliance due to outdated equipment.